

Montreux Collaborative Blog
Greater together: taking joint action to accelerate PFM reform for health
Hélène Barroy, Moritz Piatti, Jennifer Asman, Eric Boa, Rosemary Owino
Public financial management and universal health coverage
Public financial management (PFM) has emerged as a critical driver of effective health systems and outcomes. Global and regional analyses have shown that robust PFM systems are associated with reduced maternal, under-five and non-communicable disease mortality rates. Unpacking how PFM data, systems, processes, and capacity contribute to better health has been a collaborative multi-year endeavor. Since 2014, the World Health Organization has championed the Montreux Collaborative on Fiscal Space, PFM and Health Financing. This collaborative platform has facilitated knowledge production and sharing, and contributed to elevate the PFM for Health agenda from obscurity to prominence within health systems and financing policies.
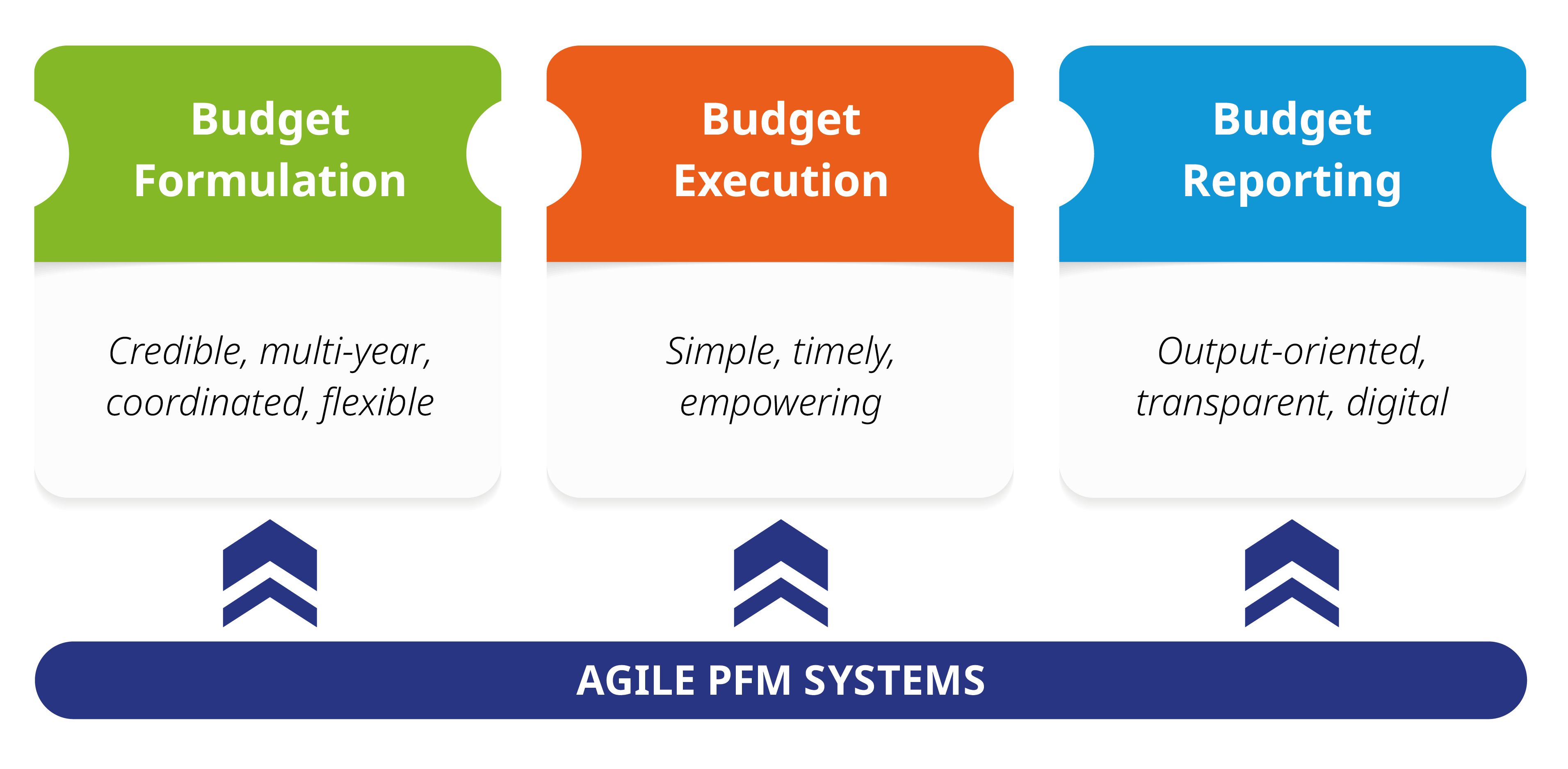
Over the past decade, extensive conceptual and analytical work has focused on adapting domestic public finance systems in low-and-middle income countries to make them more agile and responsive to the needs of UHC (see Figure 1). Assessments covered health budget formulation, credibility and budget execution practices from both health and finance perspectives. The COVID-19 pandemic has provided an opportunity to identify good practices and reforms for building emergency-responsive PFM systems. These adaptations are crucial for ensuring efficient allocation and utilization of budget resources during crises.
Recognizing the importance of country-specific context, efforts have been made to align decentralization, PFM, and health financing. This alignment aims to inform more coordinated and consistent reforms. As the agenda progresses, there is a growing emphasis on PFM issues related to health service delivery. The renewed interest in Primary Health Care (PHC) presents an opportunity to deepen guidance. This includes enhancing financial flexibility and autonomy for primary care service providers.
Figure 1. Agile and responsive PFM systems to support UHC
Public financial management and external assistance to health
The launch of the Lusaka Agenda in December 2023 renewed interest in PFM systems as a conduit for channeling external resources into health systems. Recognizing the costs associated with misaligned financial management and reporting systems, major health-sector development partners, such as the Global Fund to Fight AIDS, Tuberculosis and Malaria (the Global Fund) and Gavi, the Vaccine Alliance – are reinforcing already existing initiatives to align their grant-operating modalities with countries’ domestic PFM rules and processes. For example, Gavi aims to channel at least 55% of their non-vaccine funding through countries’ financial systems by 2025. The Global Fund and Gavi are taking a progressive and adaptable approach, considering the varying maturity levels of country systems. To achieve this, they explore collaborations with professional accountancy organizations and supreme audit institutions (such as the International Federation of Accountants and the African Association of Supreme Audit Institutions) to foster accountability and good governance of public funds in health.
This welcome shift in alignment of aid necessitates significant transformation for all parties. Development agencies must streamline their financial management requirements, while partner countries must strengthen their PFM practices. Governments need to reevaluate multiple aspects of the budget cycle. This includes how grant funding is included in health budgets, disbursed, and accounted for, reported, and audited. A shared challenge is synchronizing PFM strengthening for aid alignment with broader reforms that support UHC. Avoiding fragmentation and rigidities in health spending is crucial. Increased use of PFM systems must also be accompanied by increased use of government structures and delivery institutions to avoid perpetuating a parallel and fragmented financing system.
Collective action
As the PFM for Health agenda gains political momentum and evolves, the Montreux Collaborative is undergoing reshaping and expansion. At the November 2023 Montreux Collaborative meeting, the World Health Organization (WHO), the World Bank, and UNICEF announced a deeper collaboration. Their joint efforts aim to strengthen coordination in analysis, capacity building, and technical support related to this critical agenda.
Opportunities exist to extend this collaboration to other health-sector development partners, including the Global Fund and Gavi. Harmonizing messaging and enhancing efficiency across global, regional, and country activities are priorities. For the first time, the five organizations—WHO, World Bank, UNICEF, the Global Fund, and Gavi—will collaboratively set the agenda for the next Montreux event on Fiscal Space, PFM, and Health Financing. This event, scheduled for November 2025, will bring together global efforts to advance the knowledge agenda and drive impact on country-level reforms.
The renewed Montreux Collaborative remains committed to gathering key stakeholders and amplifying their voices. This includes governments, non-health partners (such as the OECD and IMF), peer-learning organizations (e.g., R4D, P4H, CABRI), academia (advancing systematic inclusion of PFM in health financing research), and civil society (ensuring participatory and inclusive discussions). Moving forward, the renewed Montreux platform aims to serve as a collaborative and adaptive multistakeholder coordination framework, advancing this critical agenda in support of aid alignment and overall support to UHC.
Authors affiliations: Hélène Barroy (WHO Headquarters), Moritz Piatti (World Bank Group), Jennifer Asman (UNICEF East Asia and Pacific), Eric Boa (The Global Fund to Fight AIDS, Tuberculosis and Malaria), Rosemary Owino (Gavi, the Vaccine Alliance)
Photo copyrights: Getty Images
15 July 2024